Total Knee Replacement
Osteoarthritis is the most common form of chronic arthritis. The condition affects approximately 1.4 million Australians, or approximately 7.3% of the population. The cause of osteoarthritis (OA) is not completely understood. Being overweight or obese can contribute to OA, particularly in females. Obesity is more strongly associated with OA of the knee than the hip. Individuals with a history of joint trauma or injury are more likely to develop OA. Joint injuries include dislocation, fracture, and tears of the cartilage or ligaments. Congenital abnormalities (conditions that are present at birth) can cause abnormal joint alignment, which may lead to OA. The alignment of a joint affects the load across the cartilage and other tissues. Areas of cartilage under high load or pressure can degrade faster or be damaged by joint movement. This may lead to early-onset OA. OA may run in families. A person is more likely to develop OA if their parents have OA that is early in onset or involves more than one joint.
Total knee replacement surgery was first performed in 1968. Since then, knee replacement surgeons have been using improvements in surgical materials and techniques have greatly increased its effectiveness. Total knee replacement, or total knee arthroplasty, is a surgical procedure in which parts of the knee joint are replaced with artificial parts (prostheses). Dr Singh has been performing knee replacement surgery since 2004.
Approximately 97% of total knee replacements performed in Australia are due to OA. The disease is uncommon before the age of 45 years and mostly affects people aged 65 years or over. It is more common in females than in males.
Osteoarthritis usually progresses slowly and may produce non-specific local symptoms that impair health-related quality of life, such as pain with joint use, stiffness, loss of joint mobility and function and alteration in the shape of the joint. The knee is most commonly involved, followed by the hip. The spine, foot and joints of the hand can also be affected.
Information About Knee Replacements
Total knee replacement surgery was first performed in 1968. Since then, knee replacement surgeons have been using improvements in surgical materials and techniques have greatly increased its effectiveness. Total knee replacement, or total knee arthroplasty, is a surgical procedure in which parts of the knee joint are replaced with artificial parts (prostheses). Dr Singh has been performing knee replacement surgery since 2004.
The knee is the largest joint in your body. In a normal, healthy knee, the bone surfaces that come together at the joint are smooth and hard. A cushioning layer of tissue (called articular cartilage) prevents contact between these bones. This tough layer of tissue allows the joint to move without creating friction or wear on the bone surfaces. As the cartilage breaks down, the underlying bone is often left exposed and unprotected, producing bony spurs called osteophytes. In addition, soft tissues around the joint (such as the synovium, ligaments and tendons) can become inflamed and swollen. As these changes occur, the joint loses its smooth movement, becoming stiff and painful. Reduced use of the painful joint causes the muscles to weaken and lose bulk. This in turn increases the load and damage to the cartilage, bone and soft tissues. In advanced stages of OA, the space between the bones is reduced and bones can be in direct contact during movement. This results in increased pain and further joint damage and a deterioration in the quality of life.
For more information please read our detailed guide
How long will my knee replacement last ?
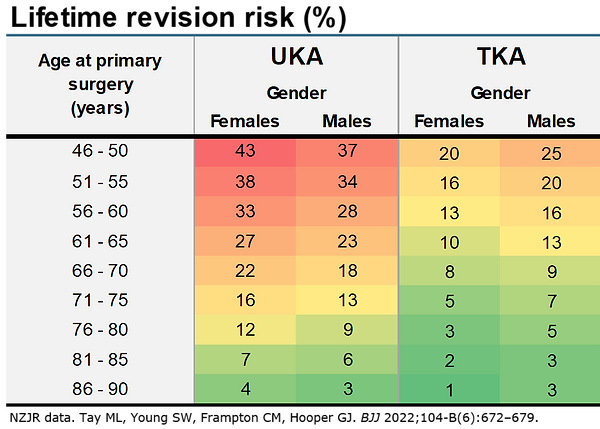
Reference Article Link https://boneandjoint.org.uk/Article/10.1302/0301-620X.104B6.BJJ-2021-1744.R1
What Is The Process Moving Forward?
Step 1: Book A Consultation
If you do require surgery, we will schedule and walk you through the process of your operation.
Step 2 Schedule Surgery
During your appointment, Dr Parminder Singh will take a history, examine you and review the relevant radiology. If any further scans are required Dr Singh will request those. Once the diagnosis has been confirmed Dr Singh will discuss the non-surgical option and surgical options of surgery. If no surgery is required Dr Singh may refer you to a physiotherapist for non-surgical management. If surgery is required Dr Singh will consent you for the surgery explained the risk and benefits of the procedure and the expected outcome.
Step 3 Surgery
Dr Parminder Singh will see you before the surgery in the waiting bay and ensure all your questions have been answered prior to surgery.
Dr Parminder Singh will examine your hip, thigh and leg making sure there are no open wounds or signs of skin infection.
If there are any signs of infection, you surgery will be cancelled and rescheduled for another day. Once this has been check Dr Parminder Singh will draw an arrow on the side of your thigh confirming with you the side of surgery. Dr Parminder Singh will check your consent form to again confirm the operation being performed and side of surgery.
Step 4 Recovery
Following you surgery, you will recover on the ward. Most individual stay one night in hospital and will be seen by the physiotherapist on the ward to facilitate mobilisation using crutches for the first 1-2 weeks.
Some individuals will use the crutches for longer depending on the type of injury and treatment required. Dr Parminder Singh will see you in his rooms approximately 10-14 days after the hip arthroscopy surgery and inspect the hip wound.
The stitches will be removed during this appointment. Dr Parminder Singh will also explain the operative findings and recommended precautions and rehabilitiation required. Another appointment will typically be organised for you around 6-8 week after this date to assesss your progress. In the meantime, rehabilitation is usually recommended with a physiotherapist who has experience with hip arthroscopy patients.
It is important to follow the hip precautions Dr Parminder Singh recommends to allow for the best possible outcome.
Any further appointement will be made on a case by case basis depending your condition. In general terms Dr Parminder Singh recommends approximately 3 months for healing from the surgery and hip precautions during this periods.
Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Make an appointment with our Melbourne orthopaedic surgeons
If you are a patient suffering from a knee or hip issue, you can get a referral and make an appointment with a surgeon at PJS Orthopaedics at a time and location that suits you.
Whether your knee or hip injury is a result of playing sport, has come about because of trauma injury, or is simply due to wear and tear, our Melbourne surgeons have the experience and expertise to find a surgery solution that is right for you.






