A Patient Guide To Femero-Acetabular Impingement (FAI) – Assessment, Investigation And Hip Arthroscopy Surgical Treatments
Written by Dr Parminder J Singh MBBS, MRCS, FRCS (Tr&Oth), MS, FRACS
Orthopaedic & Trauma Surgeon
Specialist in Hip & Knee Key Hole Surgery
Hip & Knee Replacement Surgery
Welcome to Parminder J Singh’s patient guide to femero-acetabular impingement and hip arthroscopy. The aim of this information sheet is to provide a provide Dr Parminder Singh’s patients a general guide to understanding what is femero-acetabular impingement, the assessment and investigation process and finally the hip arthroscopy surgical treatments. Every patient and every operation is unique and therefore this guide will not be able to answer all your questions. This guide is not a substitute for obtaining medical advice from your surgeon. However, this guide may assist you to get a better understanding of what to expect and it may help you think of questions to ask Dr Parminder Singh. If this patient information guide does not answer your questions, remember that Dr Parminder Singh will do his best to do so at your consultation. Dr Singh and his surgical team will practice in accordance with the ethical standards defined by the Australian Medical Council.
 Introduction
Introduction
Arthroscopic (keyhole) examination of cadaveric hips was first described by Burman in 1931. Up until 2003, hip arthroscopy was a procedure undertaken mainly for diagnostic purposes and basic interventions such as removal of loose bodies and debridement of damaged tissue such as the acetabular labrum. Since the scientific publication of Dr Reinhold Ganz’s work on femoro-acetabular impingement in 2003, orthopaedic surgeons have developed both open and arthroscopic strategies to address the damage caused by these mechanisms. With growing recognition and evidence of the efficacy and benefits of these interventions it has also become apparent that arthroscopic interventions achieve comparable outcomes, with less morbidity.
Arthoscopic Anatomy
The hip joint comprises central (green) and peripheral (yellow) compartments which are separated by the acetabular labrum (blue). (Figure 1)
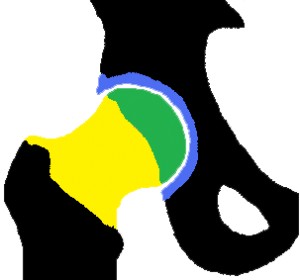
FIGURE 1: CENTRAL AND PERIPHERAL COMPARTMENT OF THE HIP JOINT
The lateral compartment is deep to the tensor fascia lata (black line). Arthroscopic access to this space allows visualisation and interventions to the trochanteric bursa (pink) and gluteus medius (maroon) and minimus (red) tendons.
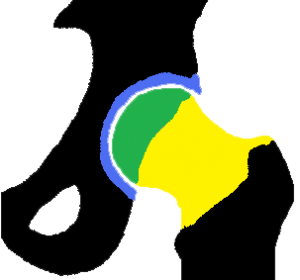
FIGURE 2: LATERAL COMPARTMENT OF THE HIP JOINT
 Indications For Hip Arthroscopy
Indications For Hip Arthroscopy
Dr Parminder J Singh’s current indications for hip arthroscopy include the presence of symptomatic femero-acetabular impingement with cam lesions and or labral tears, chondral(cartilage) lesions, osteochondritis dissecans (cracks in the underlying cartilage and or bone), ligamentum teres injuries (tears) , snapping hip syndrome ( painful clicking iliopsoas tendon or ilio-tibial band), iliopsoas bursitis, unexplained symptomatic total hip replacement (occasionally indicated) and removal of loose bodies.
Less common indications include management of osteonecrosis (loss of blood supply) of the femoral head, synovial (inner surface of hip lining) abnormalities, crystalline hip arthropathy (gout and pseudogout), infection and post-traumatic haematomas (blood clots) and intra-articular (in the hip joint) debris.
Some hip arthroscopists have noted that the symptoms of mild-to-moderate hip osteoarthritis (> 2mm of joint space) can be temporised; particularly when peripheral osteophytes (bone spurs) are causing mechanical symptoms. The benefit and duration of improvement are variable and need to be selected on a case by case basis. In the presence of <2mm joint space, hip arthroscopy is more likely not to provide a significant benefits.
 Description Of Femoro Acetabular Impingement
Description Of Femoro Acetabular Impingement
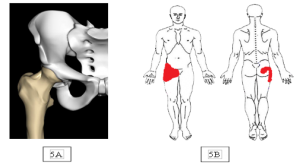
Dr Parminder J Singh most commonly see’s two distinctive types of femoro-acetabular impingement (FAI) are recognised. “Pincer impingement” occurs as a result of anterior over coverage (red triangle figure B) of the acetabulum (socket) or acetabular retroversion causing abutment against the femoral head neck junction during hip flexion (figure c) causing damage to the hip joint particular the acetabular labrum.
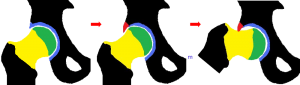
“Cam impingement” occurs when a non-spherical femoral head (red semi-circle see figure B) abuts against the anterior acetabulum (C), usually with the hip in flexion causing damage to the hip joint, particularly the cartilage and labrum.
FIGURE:4
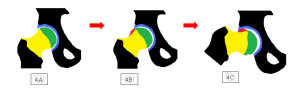
In practice it is common to see a mixed Cam and Pincer pathology, occurring along the anterior femoral neck and the anterior superior acetabular rim.
CLINICAL PRESENTATION
Patients with hip impingement typically present with pain in the groin region, side of their hip and or deep buttock pain. Impingement pain can be associated with lower back and or pubic discomfort and often tightness in the adductors (inner thigh muscles), Tensor fascia lata (muscle sheet on side of hip), Rectus femoris tendon (tendon at front of groin) and or the iliopsoas muscle.
In patients where cam impingement predominates, symptoms are often precipitated by prolonged upright sitting and internal rotation movement in flexion. An examination of the hip joint will often reveal asymmetric ranges of movement and evidence of irritability. Cases of Cam impingement typically show reduced internal rotation of the hip in flexion. This may be bilateral. Specific tests Dr Parminder J Singh will perform for impingement are:
FADIR TEST
With the hip in high flexion, adduction and internal rotation (FADIR), abutment and impingement of the labrum and cartilage occurs. Figures 6 B and C.
FIGURE 6:

FABER TEST
With the hip in flexion, abduction and external rotation (FABER), abutment of the abutment of the labrum and cartilage also can occur. Figure 7 B and C
FIGURE 7:

Where pincer type impingement predominates, abduction and external rotation movements may be more troublesome. A significant proportion of female patients with impingement will report exacerbation of their symptoms during sexual intercourse. In cases of pincer type impingement ranges of movement may appear normal but with pain towards the extremes of movement.
Athletes, sportsmen, sportswomen and dancers typically describe pain on training and early fatigue. These symptoms will improve with rest but always recur on resumption of exercise.
 Investigations
Investigations
PLAIN RADIOGRAPHS
Dr Parminder J Singh will typically review or request plain X-rays of the hips. These should comprise an anterior posterior (AP) standing view of both hips, a standard lateral of the affected hip and a Dunn view of the affected hip. The AP view should be assessed both for degenerative changes and also evidence of the Cam type deformity shown in Figure 1a and the Profunda socket shown in Figure 1b, as well as the crossover sign indicating a prominent anterior acetabular wall, or acetabular retroversion.
FIGURE 8:

MRI SCANS
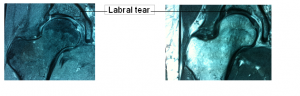
Where Dr Parminder J Singh suspects any labral pathology, damage to the acetabular cartilage or ligamentum teres, a MRI scan is the preferred investigation (see Figure 9)
FIGURE 9: MRI SHOWING LABRAL TEAR
Pritchard O’Donnell (POD) CT Scan
Where the shape if the femoral head neck junction needs to be assessed for the presence of a Cam deformity, CT 3D surface reconstructions allow the lesion to visualised and surgical resection planned, Figure 10.
FIGURE 10: CT 3D RECONSTRUCTION SCAN SHOWING CAM LESION

Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
Brighton VIC 3186
Book a consultation on:
(03) 9428 4128
Boxhill VIC 3128
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
Blanton Dr,
Mulgrave VIC 3170
Book a consultation on:
(03) 9428 4128
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Make an appointment with our Melbourne orthopaedic surgeons
If you are a Melbourne patient suffering from a knee or hip complaint, you can get a referral and make an appointment with a surgeon at PJS Orthopaedics at a time and location that suits you.
Whether your knee or hip injury is a result of playing sport, has come about because of trauma injury, or is simply due to wear and tear, our Melbourne surgeons have the experience and expertise to find a surgery solution that is right for you.






