Dr Parminder J Singh treats a number of conditions affecting the hip joint leading to groin pain (including impingement of the hip and labral tears) and lateral hip pain (also known as greater trochanteric pain syndrome) using hip arthroscopy techniques. One of the common causes of groin pain, lateral hip pain, and or buttock pain is femeroacetabular impingement leading to a labral hip tear.
Impingement of the hip leading to a symptomatic labral hip tear, may well require consideration for treatment. The surgical treatment for a labral tear in hip may require a hip arthroscopy and labral repair. Consideration also should be given to the cause of the torn hip labrum and potential correction of any hip impingement.
Another cause of lateral hip pain that it is particularly common in female between the ages of 40 and 60 is known as greater trochanteric pain syndrome. Individuals failing to improves with physiotherapy, steroids, and plates rich plasma (prp), can be treated using arthroscopic techniques ( hip arthroscopy).
Dr Parminder J Singh recently published his randomized control study showing up to 70% improvement in symptoms following hip arthroscopy.
Patient Guide To Femero-Acetabular Impingement And Hip Arthroscopy
The aim of this information sheet is to provide Mr Parminder Singh’s patients a general guide to understanding what is femero-acetabular impingement, the assessment and investigation process and finally the hip arthroscopy surgical treatments.
Every patient and every operation is unique and therefore this guide will not be able to answer all your questions.
This guide is not a substitute for obtaining medical advice from your surgeon. However, this guide may assist you to get a better understanding of what to expect from your hip arthroscopy surgery and it may help you think of questions to ask Mr Parminder Singh. If this patient information guide does not answer your questions, remember that Mr Parminder Singh will do his best to do so at your consultation. Mr Singh and his surgical team will practice in accordance with the ethical standards defined by the Australian Medical Council.
What Is Hip Arthroscopy?
Hip arthroscopy is a minimally invasive surgical procedure that allows visualisation of the hip joint via a telescope type device known as an arthroscope via 1-2cm key holes incisions through the skin.
During the hip arthroscopy procedure, the surgeon will be able to assess the condition of hip joint, diagnose, potentially treat hip injuries and disease.
Why Would I Need Hip Arthroscopy Surgery ?
Individuals affected with symptomatic femero-acetabular impingement have been identified as at increased risk of developing arthritis in the hip joint.
Early intervention in the form of hip arthroscopy is an option of treatment that can help improve the symptoms, individuals often get with femero-acetabular impingement. Long term studies (>10 years) are awaited to see if the arthritis process can be prevented or delayed.
Patients typically will suffer from the following symptoms:
- Pain located in the groin
- Associated pain particularly in the buttock, side of the hip (lateral hip pain) , inside of thigh (adductors) and thigh region
- Pain during activities walking, sitting to standing, running and twisting
- Pain that has not improved with medicine and or physiotherapy for at least three months
- Athletes, sportsmen, sportswomen and dancers typically describe pain on training and early fatigue. These symptoms will improve with rest but often recur on resumption of exercise.
What Conditions Does Hip Arthroscopy Surgery Treat?
Mr Parminder Singh most commonly see’s two distinctive types of femoro-acetabular impingement (FAI) are recognised. In practice it is common to see a mixed Cam and Pincer pathology, occurring along the anterior femoral neck and the anterior–superior acetabular rim.
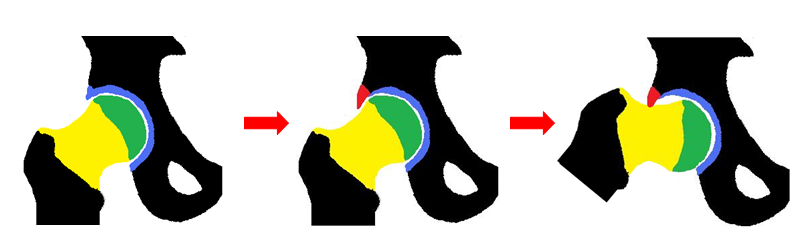
Pincer Impingement
Occurs as a result of anterior over coverage (red triangle –figure B) of the acetabulum (socket) or acetabular retroversion causing abutment against the femoral head neck junction during hip flexion (figure c) causing damage to the hip joint particular the acetabular labrum
Where pincer type impingement predominates, abduction and external rotation movements may be more troublesome. A significant proportion of female patients with impingement will report exacerbation of their symptoms during sexual intercourse. In cases of pincer type impingement ranges of movement may appear normal but with pain towards the extremes of movement.
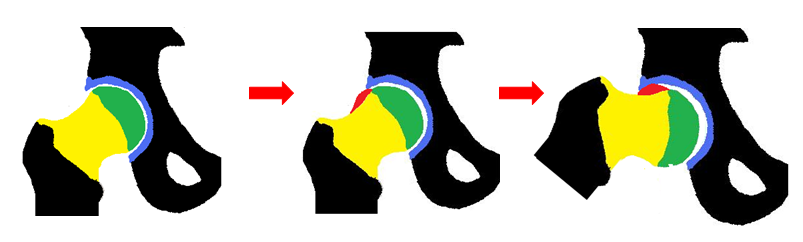
Cam Impingement
Occurs when a non-spherical femoral head (red semi-circle see figure B) abuts against the anterior acetabulum (C), usually with the hip in flexion causing damage to the hip joint, particularly the cartilage and labrum. In patients where cam impingement predominates, symptoms are often precipitated by prolonged upright sitting and internal rotation movement in flexion.
An examination of the hip joint will often reveal asymmetric ranges of movement and evidence of irritability. Cases of large Cam impingement typically show reduced internal rotation of the hip in flexion. A portion of individual will have the condition affecting both hips.
Other Conditions Hip Arthroscopy Treats:
- Acetabular labral tears
- Femero-acetabular impingement (FAI)
- Cartilage Repair
- Ligamentum teres tears
- Synovitis
- Early arthritis in selected cases
- Losse bodies
- Synivial chondromatosis
- Gluteal tendinopthy
- Trochanteric Bursitis
- Great trochanteric pain syndrome
- Snapping hip including snapping iliotibial band and iliopsoas
- Pain total hip replacement in selected cases
What Is The Process Moving Forward?
Step 1: Book A Consultation
If you do require surgery, we will schedule and walk you through the process of your operation.
Step 2 Schedule Surgery
During your appointment, Dr Parminder Singh will take a history, examine you and review the relevant radiology. If any further scans are required Dr Singh will request those. Once the diagnosis has been confirmed Dr Singh will discuss the non-surgical option and surgical options of surgery. If no surgery is required Dr Singh may refer you to a physiotherapist for non-surgical management. If surgery is required Dr Singh will consent you for the surgery explained the risk and benefits of the procedure and the expected outcome.
Step 3 Surgery
Dr Parminder Singh will see you before the surgery in the waiting bay and ensure all your questions have been answered prior to surgery.
Dr Parminder Singh will examine your hip, thigh and leg making sure there are no open wounds or signs of skin infection.
If there are any signs of infection, you surgery will be cancelled and rescheduled for another day. Once this has been check Dr Parminder Singh will draw an arrow on the side of your thigh confirming with you the side of surgery. Dr Parminder Singh will check your consent form to again confirm the operation being performed and side of surgery.
Step 4 Recovery
Following your surgery, you will recover on the ward. Most individual stay one night in the hospital and will be seen by the physiotherapist on the ward to facilitate mobilisation using crutches for the first 1-2 weeks.
Some individuals will use the crutches for longer depending on the type of injury and treatment required. Dr Parminder Singh will see you in his rooms approximately 10-14 days after the hip arthroscopy surgery and inspect the hip wound.
The stitches will be removed during this appointment. Dr Parminder Singh will also explain the operative findings and recommended precautions and rehabilitation required. Another appointment will typically be organised for you around 6-8 week after this date to assess your progress. In the meantime, rehabilitation is usually recommended with a physiotherapist who has experience with hip arthroscopy patients.
It is important to follow the hip precautions Dr Parminder Singh recommends to allow for the best possible outcome.
Any further appointment will be made on a case by case basis depending on your condition. In general terms, Dr Parminder Singh recommends approximately 3 months for healing from the surgery and hip precautions during this period.
For Further Information Please Refer To Dr Parminder J Singh’s Patient Guides
Expert hip diagnosis and treatment. Focused on you. Dr Parminder J Singh provides quality patient advice and care in the field of orthopaedics.
Click here to view all patient guides.
Frequently Asked Questions About Hip Arthroscopy?
Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Make an appointment with our Melbourne orthopaedic surgeons
If you are a patient suffering from a knee or hip issue, you can get a referral and make an appointment with a surgeon at PJS Orthopaedics at a time and location that suits you.
Whether your knee or hip injury is a result of playing sport, has come about because of trauma injury, or is simply due to wear and tear, our Melbourne surgeons have the experience and expertise to find a surgery solution that is right for you.