 Patient Guide To Total Hip Replacement
Patient Guide To Total Hip Replacement
Written by Dr Parminder J Singh MBBS, MRCS, FRCS (Tr&Oth), MS, FRACS
Welcome to Parminder J Singh’s patient guide to Total Hip Replacement. To help assist in your recovery, it is important for you to know about the surgery prior to you arriving to St Vincent’s Private East Melbourne or Epworth Eastern Private Hospital, Epworth Richmond Private Hospital or Waverly Private Hospital.
This guide is designed for patients who have already decided to have joint replacement surgery. Every patient and every operation is unique and therefore this guide will not be able to answer all your questions. This guide is not a substitute for obtaining medical advice from your surgeon. However, this guide may assist you to get a better understanding of what to expect and it may help you think of questions to ask Dr Parminder Singh. If this patient information guide does not answer your questions, remember that Dr Parminder Singh will do his best to do so at your consultation. Dr Singh and his surgical team will practice in accordance with the ethical standards defined by the Australian Medical Council.

AIM OF THE TOTAL HIP REPLACEMENT
The principle aims of the hip replacement are to reduce your pain, correct any deformity, enhance your mobility that is impeded by your hip and improve the quality of your life. This can be achieved in up to 95% of cases. The hip replacement involves replacing a hip joint that has been damaged or worn away, usually by arthritis or injury.
WHAT IS ARTHRITIS?
Osteoarthritis is characterised by joint pain and mobility impairment associated with the gradual wearing of cartilage. The wear and tear of the joint frequently results in pain, stiffness and reduced movement. The clinical diagnosis is usually based on the presence of joint symptoms and evidence of a reduction of joint space seen on the x-ray. There are different types of arthritis causing joint pain for example osteoarthritis, rheumatoid arthritis and post traumatic arthritis.
HOW COMMON IS ARTHRITIS?
Osteoarthritis is the most common form of chronic arthritis. The condition affects approximately 1.4 million Australians, or approximately 7.3% of the population. The prevalence of osteoarthritis increases with age. Osteoarthritis most commonly develops between the ages of 45 to 90 years. The pain and disability associated with osteoarthritis affects approximately 10% of men and 18% of women over 60 years of age. The incidence and prevalence of osteoarthritis will continue to rise as the population ages. The hip is the second most commonly affected joint in the body.

THE HIP JOINT
The hip joint is a ball and socket joint. The hip joint allows movement to occur between the thigh bone (femur) and the hip bone (pelvis). The pelvis contains the socket (acetabulum) and the ball shaped head of the femur fits into the acetabulum.
The outer surface of the femoral head and the inside surface of the acetabulum are covered with cartilage which allows low friction free movement between the two surfaces. The hip joint is covered by ligaments that help stabilise the joint. The hip joint movements are initiated and controlled by the muscles in the buttock, groin and thigh.
 Hip Joint Replacement
Hip Joint Replacement
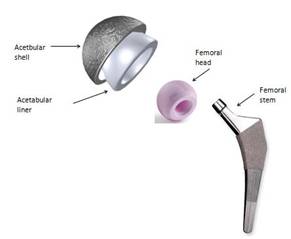
Approximately 20,000 primary total hip replacements are performed in Australia. Each hip prosthesis is made up of several components. The acetabular component replaces the acetabulum (socket). The acetabular component is typically made of a metal alloy outer shell with a fitted plastic (polyethylene) or ceramic liner or it can be made completely of one polyethylene component.
The femoral component replaces the femoral head. The femoral component is typically a two piece design. This comprises the femoral stem made of a metal alloy and the femoral head that attaches to the stem. The femoral head can be made of either ceramic or metal alloy.
 Prior To Surgery
Prior To Surgery
- Consultation with Dr Parminder Singh – Dr Singh will take a history and examine your hip and relevant x-rays during your initial consultation. Dr Singh will discuss the diagnosis, non-operative and operative options of treatment. Generally Dr Singh will discuss total hip replacement surgery if you have failed to improve with non-operative measures. Non operative measures include taking painkillers or anti-inflammatories or using physical aids like a walking stick.
- Should you wish to pursue surgery Dr Singh will decide on the type surgical approach (anterior minimally invasive muscle sparing or mini posterior approach) and the implants for your hip replacement. Dr Singh will explain to all his patients the risks and benefits of the operation in understandable language
- Consultation with your peri-operative physician – A pre-operative assessment will be undertaken one of Dr Singh’s physicians and any significant health problems should be corrected as far as possible before your hip replacement.
- Consultation with your anaesthetist – Dr Singh’s anaesthetics will contact you either prior to your surgery or on the day of your surgery to discuss the best type of anaesthetic for you. Depending on the time day the surgery will be undertake will determine the time you stop eating and drinking to ensure a safe anaesthetic. Generally you will be advised no food or drink 6 hours prior to your surgery.
Your hospital admission
- On the day of your total hip replacement, you will be checked in by the staff on the ward. Once you are in waiting bay for surgery, Dr Singh and his team will meet you and mark the operated leg to confirm the site of surgery. A series of checks will be undertaken following the World Health Organisation guidelines to ensure a safe entry into the operating room.
 Your Operation
Your Operation
Dr Singh will discuss the best way to implant your hip replacement based on your individual circumstances. Dr Singh can implant your hip replacement with through the front of your hip using the minimally invasive muscle sparing anterior approach or through the mini-posterior approach. Usually both techniques work very well with excellent outcomes.
During your surgery Dr Parminder Singh will replace your hip joint with the artificial hip replacement. Dr Singh will insert a pain catheter into your hip joint which will help reduce your post-operative pain and potential reduce your morphine requirements. This should make you feel less nausea following your surgery and potentially allow you the opportunity to mobilise sooner after your hip replacement. Your wound will be covered with a waterproof dressing.
YOUR POST-OPERATIVE RECOVERY
The pain pump will be removed 24 hours after your surgery. Generally the physiotherapy will assist with your mobilisation on the same day or the following day after your surgery. Dr Singh and the peri-operative physician will see you after the surgery and coordinate a safe and smooth recovery. Check blood test will be undertaken the following day, 2 post-operative doses of antibiotics will be administered 8 and 16 hours after your surgery. A routine post-operative x-ray will be requested for Dr Singh to review he is satisfied with the position of the hip replacement components. Patients tend to either go home directly or to a rehabilitation service depending on your individual personal circumstances. On average, patients will go home after 3-5 days after their surgery. No one will be sent home until the patient feels safe and confident to mobilise safely. You will be advised by the physiotherapist to avoid crossing your legs or twisting your hip inwards and outwards particular during the first 6 weeks. Most patients will develop swelling and bruising around the thigh and operative site, by using an intermittent ice pack can help assist sooth the operative site and reduce swelling.
 Complications Of Total Hip Replacement
Complications Of Total Hip Replacement
Most of the time complications do not occur. However, every operation has risks. These can be related to the anaesthetic itself or to the surgery. Anaesthetic complications are rare and include unexpected reaction to the anaesthetic. During the surgery there is a risk of excessive bleeding or injury to a nerve or major blood vessel. There is also a risk of developing a blood clot following total hip replacement surgery.
-
- Infection – to reduce the risk Dr Singh will prescribe antibiotics for you to take at the time of your surgery and also two post-operative doses of antibiotics 8 and 16 hours after your surgery.
- Dislocation – this is most likely to occur in the first 6 weeks after your surgery and may need another procedure to treat this. You will be advised of hip precautions to take by your physiotherapist to reduce the risk.
- Leg length discrepancy – your leg may be slightly shorter or longer after your hip replacement and the difference in leg length can be corrected by wearing a shoe raise on the short side to correct the discrepancy.
-
-
- Hip fracture (peri-prosthetic fracture) – tiny cracks can occur in your bone when implanting your new hip replacement. They usually heal on their own, however sometimes a fracture may require further surgery.
- Nerve damage – it is quite common to get some numbness around your scar, however, rarely the sciatic nerve may be stretched and can result in either temporary (usually) or permanent (rarely) weakness in the foot.
-
 Preparing Your Home Following Your Hip Replacement
Preparing Your Home Following Your Hip Replacement
When you return home, you will experience some initial temporary restricted mobility that will eventually recover. Some modifications you might consider to your home to make the early transition easier and safer include:
WALKWAYS
Remove loose rugs to avoid tripping. If the rugs cannot be removed consider the application of a non-skid backing.
TOILETS
You will need to toilet seat raise for the first six week to reduce the risk of your hip dislocating after your surgery.
STAIRS
You may find it easier for the first six weeks to move your bed downstairs onto the ground floor particular if you find it difficult to ascend and descend stairs.
 Post-Operative Review
Post-Operative Review
Dr Parminder Singh’s secretary will organise a post-operative wound review approximately 10-14 days following your surgery. Dr Singh will inspect your wound during this appointment and remove stiches or staples. This will be an opportunity for you to ask any further questions. A further appointment will be organised for you at approximately 6-8 weeks later to assess your progress. Generally, you are likely to be walking with either one or no sticks at this stage and safe to return to work and driving.
You hip replacement will continue to heal over the course of the next 12 -18 months and Dr Singh will organise to see you at 6 months and 12 months after your surgery. At these appointments, Dr Singh will organise x-rays to assess how the bony is attaching to the components inserted into your hip.
PHYSIOTHERAPY FOLLOWING YOUR TOTAL HIP REPLACEMENT GUIDELINES
Dr Parminder Singh recommends working closely with an experienced physiotherapist will facilitate your rehabilitations and improve your confidence and strength back in your hip. Patients will vary how much time they will spend in hospital and the speed at which they achieve their milestones in the recovery pathway for a total hip replacement. Dr Parminder Singh however, generally recommends early mobilisation to help reduce complications of sitting in bed.
 Tips after your hip operation to reduce risk of dislocation
Tips after your hip operation to reduce risk of dislocation
The following precautions are important to reduce the risk of dislocation. They should be followed particularly during the first 6 weeks after your hip replacement.

1. Do not bend your hip greater than 90 degrees.
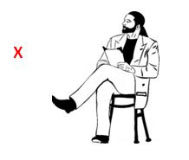
2. Do not cross your legs.
3. Do not twist on your operated leg when turning

4. Do not bend over too much to pick things off the floor.
5. When sleeping, attempt to sleep on your back and avoid crossing over your legs. Putting a pillow between your legs may assist you in this. Generally aim to do this for approximately 6 weeks after your surgery.
 Tips For Your Hip
Tips For Your Hip
- Generally, the hospital physiotherapist will visit you on the day or morning after your surgery. They will check Dr Parminder J Singh post-operative instructions and work with you closely over the next few days. Initially, the physiotherapist will help you take a few steps to sit in the chair. You will be provided with a walking frame to help you balance and you will be advise to weight bear as per Dr Singh post operative instructions – usually full weight bearing.
- When walking, you will need to know how to turn around and change direction – remember not to pivot or twist on your operated leg; step around instead. You will progress the distance you walk daily and walk up and down the isle of the ward.
 Some Tips For Sitting And Standing
Some Tips For Sitting And Standing
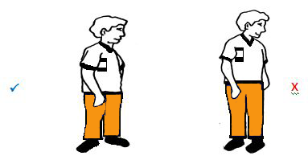
STANDING UP:
Move to the edge of your chair; push up using the arms of your chair to facilitate standing.
SITTING DOWN:
Initially, make sure you can feel the back of the chair against the back of your legs. Then reach back for the arms of the chair. Without leaning forward, gently lower yourself into your chair, taking the weight evenly through your arms. You may find it more comfortable to slide your operated leg forwards as you sit down.

 Some Tips For Ascending And Descending Stairs
Some Tips For Ascending And Descending Stairs
STAIRS (GOING UP)
Non operated leg first → Operated leg second → Crutch / stick third
STAIRS (GOING DOWN)
Crutch / Stick → Operated leg → Non operated leg
 Frequently Asked Questions
Frequently Asked Questions
Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Make an appointment with our Melbourne orthopaedic surgeons
If you are a patient suffering from a knee or hip issue, you can get a referral and make an appointment with a surgeon at PJS Orthopaedics at a time and location that suits you.
Whether your knee or hip injury is a result of playing sport, has come about because of trauma injury, or is simply due to wear and tear, our Melbourne surgeons have the experience and expertise to find a surgery solution that is right for you.


