Welcome to Dr. Parminder J. Singh’s Patient Guide to Total Hip Replacement in Melbourne.
Hip replacement is a highly effective and safe procedure that can reduce your pain and help you get back to your routine activities. However, Dr. Parminder Singh believes that to assist in your recovery following your hip replacement surgery, it is important for you to know about the surgery prior to arriving at either St Vincent’s Private East Melbourne, Epworth Eastern Private Hospital, Epworth Richmond Private Hospital, Waverly Private Hospital, or the Bays Hospital.
Cost of Hip Replacement Surgery
The overall cost of a hip replacement surgery is inclusive of the surgeon’s fees, hospital fees, anaesthetist fees, and surgical assistant fees.
Surgeon’s fees: Dr. Parminder Singh follows the Australian Medical Association’s (AMA) fee guidelines for all of his surgeries.
Hospital fees: This cost is covered entirely by your private health insurance. If you are uninsured, our staff will assist you with providing an estimated quote for your hip replacement surgery.
Anaesthetist and Surgical Assistant Fees: Dr. Parminder Singh has his own team of assistants and anaesthetists who also follow the AMA guidelines.
Following the consultation with Dr. Parminder Singh, a member of our staff will go over the specific costs associated with your hip replacement in Melbourne.
PATIENT’S GUIDE TO HIP REPLACEMENT SURGERY
This guide is designed for patients who have already decided to have joint replacement surgery. Because every patient and procedure is unique, this guide cannot fully address all of your enquiries. This manual is not a substitute for obtaining medical advice from your surgeon. However, by reading this guide, you may be better able to anticipate what will happen and come up with questions for Mr. Parminder Singh. Remember that Mr. Parminder Singh will make an effort to address any questions you may have during your consultation if this patient information guide fails to adequately address them. Mr. Singh and his surgical team will practise in accordance with the ethical standards defined by the Australian Medical Council.
Aim of Hip Replacement
The principle aim of hip replacement is to reduce your pain, correct any deformity, restore mobility that is impeded by your hip, and enhance the quality of your life. This can be achieved in up to 95% of cases. A hip replacement in Melbourne involves replacing a hip joint that has been damaged or worn away, usually by arthritis or injury.
For further information, please refer to Dr. Parminder Singh’s Hip Replacement Guide.
WHAT IS ARTHRITIS?
Osteoarthritis is characterised by joint pain and mobility impairment associated with the gradual wearing of cartilage. The wear and tear of the joint frequently results in pain, stiffness, and reduced movement. The clinical diagnosis is usually based on the presence of joint symptoms and evidence of a reduction of joint space seen on the x-ray. There are different types of arthritis that cause joint pain, for example, osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.


HOW COMMON IS ARTHRITIS?
Osteoarthritis is the most common form of chronic arthritis, and the hip is the second most commonly affected joint in the body. The condition affects approximately 1.4 million Australians, or approximately 7.3% of the population. The prevalence of osteoarthritis increases with age. Osteoarthritis most commonly develops between the ages of 45 and 90. Less commonly, osteoarthritis occurs under the age of 45 and may well be associated with an underlying risk factor for the development of premature arthritis. The pain and disability associated with osteoarthritis affect approximately 10% of men and 18% of women over 60 years of age. The incidence and prevalence of osteoarthritis will continue to rise as the population ages.
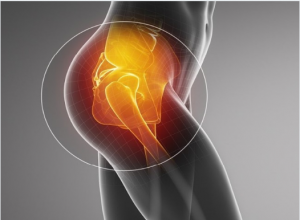
THE HIP JOINT
The hip joint is a ball-and-socket joint. The hip joint allows movement to occur between the thigh bone (femur) and the hip bone (pelvis). The pelvis contains the socket (acetabulum), and the ball-shaped head of the femur fits into the acetabulum.
The hip joint allows movement to occur between the thigh bone (femur) and the hip bone (pelvis). The pelvis contains the socket (acetabulum), and the ball-shaped head of the femur fits into the acetabulum.
FEMORAL HEAD
The outer surface of the femoral head and the inside surface of the acetabulum are covered with cartilage, which allows low-friction movement between the two surfaces. The hip joint is covered by ligaments that help stabilise the joint. The hip joint movements are initiated and controlled by the muscles in the buttock, groyne, and thigh.
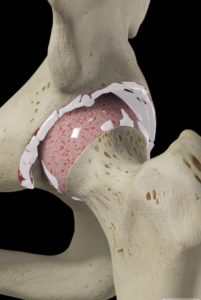
 HIP JOINT REPLACEMENT
HIP JOINT REPLACEMENT
Approximately 20,000 primary total hip replacements are performed in Australia. Each hip prosthesis is made up of several components. The acetabular component replaces the acetabulum (socket). The acetabular component is typically made of a metal alloy outer shell with a fitted plastic (polythene) or ceramic liner, or it can be made completely of one polythene component.
The femoral component replaces the femoral head. The femoral component is typically a two-piece design. This comprises the femoral stem, made of a metal alloy, and the femoral head that attaches to the stem. The femoral head can be made of either ceramic or a metal alloy.
Having performed many hip replacement procedures, Dr. Parminder J. Singh is highly adept. He will guide you through each stage, including preoperative instruction, postoperative care, and physical therapy. Get in touch with him right away if you want to get back to your regular lives!
Frequently Asked Questions About Hip Replacement?
What Is The Process Moving Forward?
Step 1: Book A Consultation
If you do require surgery, we will schedule and walk you through the process of your operation.
Step 2 Schedule Surgery
During your appointment, Dr Parminder Singh will take a history, examine you and review the relevant radiology. If any further scans are required Dr Singh will request those. Once the diagnosis has been confirmed Dr Singh will discuss the non-surgical option and surgical options of surgery. If no surgery is required Dr Singh may refer you to a physiotherapist for non-surgical management. If surgery is required Dr Singh will consent you for the surgery explained the risk and benefits of the procedure and the expected outcome.
Step 3 Surgery
Dr Parminder Singh will see you before the surgery in the waiting bay and ensure all your questions have been answered prior to surgery.
Dr Parminder Singh will examine your hip, thigh and leg making sure there are no open wounds or signs of skin infection.
If there are any signs of infection, you surgery will be cancelled and rescheduled for another day. Once this has been check Dr Parminder Singh will draw an arrow on the side of your thigh confirming with you the side of surgery. Dr Parminder Singh will check your consent form to again confirm the operation being performed and side of surgery.
Step 4 Recovery
Following your surgery, you will recover on the ward. Most individual stay three to four nights in the hospital and will be seen by the physiotherapist on the ward to facilitate mobilisation using crutches for the first 1-2 weeks.
Some individuals will use the crutches for longer depending on the type of injury and treatment required. Dr Parminder Singh will see you in his rooms approximately 10-14 days after the hip replacement surgery and inspect the hip wound.
The stitches will be removed during this appointment. Dr Parminder Singh will also explain the operative findings and recommended precautions and rehabilitation required. Another appointment will typically be organised for you around 6-8 week after this date to assess your progress. In the meantime, rehabilitation is usually recommended with a physiotherapist who has experience with hip replacement patients.
It is important to follow the hip precautions Dr Parminder Singh recommends to allow for the best possible outcome.
Further appointments will be made at approximately 6 and 12months post operatively and check x-rays will be requested. Dr Parminder Singh recommends to allow approximately 3 months for the soft tissue healing from the surgery and hip precautions during this period. The bone healing will continue for up to 12 months after surgery and Dr Singh will check this for you during the following up appointments. In terms of longer term, Dr Singh will review you in 5, 10, 15, 20 years after your hip replacement with regular x-rays.
Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
Brighton VIC 3186
Book a consultation on:
(03) 9428 4128
Boxhill VIC 3128
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
Blanton Dr,
Mulgrave VIC 3170
Book a consultation on:
(03) 9428 4128
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Book a Consultation
Committed to improving the quality of patient advice, treatment and care in the field of orthopaedics, book a one-on-one consultation with Dr Parminder J Singh today.