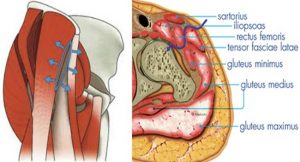
Figure 1: Anterior Approach to the hip joint
The anterior approach is a surgical technique used to approach the hip joint in an individual with arthritis. The anterior approach is commonly used to perform a total hip replacement and is considered a minimally invasive technique. This procedure also does not require the surgeon to cut any muscles and simply goes in between muscle planes (see figure 1)
Careful selection of the patients based on their anatomy, shape of their thigh and severity of arthritis can minimize complications via the anterior approach. Dr. Parminder J Singh, has received specialist fellowship training using the Anterior Approach under during his fellowship with Professor John O’Donnell in Melbourne in 2008. Dr. Singh has been performing anterior hip replacement for this Melbourne patients regularly since then.
Since 2008, the anterior hip replacement is being used more frequently in Australia. In the USA, 15-20% of the hip replacements are being undertaken via the anterior approach. The Australian National Joint Registry started collecting the surgical approach data in 2015 and reported that 37% of joint replacement in Australia were being undertaken via the Anterior Approach (see figure 2)
The most common indication for an anterior hip replacement is osteoarthritis. Individuals with advanced osteoarthritis typically will have pain in the groin, lateral hip (side of the hip), buttock and or thigh. This pain can be associated with stiffness in their hip movements. Often the ability of the patient to undertake activities of daily living becomes increasingly more difficult. Some patients walk with a limp and find it difficult to stand on one leg. During your consultation with Dr. Parminder J Singh, he will assess your leg length and range of motion, among other things. Individuals with advanced osteoarthritis will have a restricted range of motion particular with internal rotation (IR) and external rotation (ER) (See figure 3)
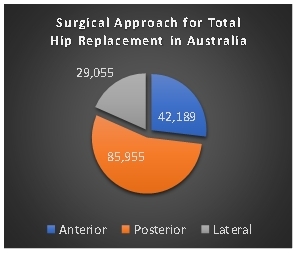
Figure 2: Chart to show the surgical approach used to replace the hip in Australia

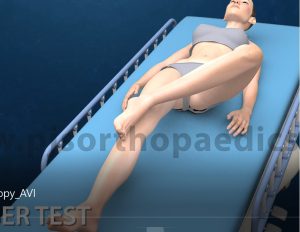
Figure 3: Clinical examination showing the internal and external rotation test
Radiological assessment of osteoarthritis often reveals some signs of loss of joint space, osteophytes (bone spurs), subchondral sclerosis and in some advanced cases sub chondral cyst formation (see figure 4)
Following a review with Dr. Parminder J Singh, which will include your medical history, clinical examination and radiological assessment, a decision will be made whether a hip replacement is indicated. Dr Parminder J Singh, will tailor his decision to determine the surgical approach and the type of hip replacement for you.
Dr. Singh in 2021 published his 5 years results in a prospective randomized control study comparing the anterior vs the posterior approach in hip replacement. The research demonstrated there was no difference in the functional, radiographic and survivorship outcomes between the direct anterior or posterior approach for hip replacements in Australia. These results are similar to other studies published around the world.
While in hospital post surgery, patients typical spend approximately 3 days in hospital prior to being discharged. Dr. Singh usually checks in on his patients approximately 10-14 days following surgery, to assess the healing of the wound and remove any stitches. Most of the patients come off their crutches in around 2-4 weeks post surgery. They would need to undergo some physiotherapy to support them during recovery. Dr. Parminder J Singh will monitor each patient’s recovery at regular, scheduled intervals and offer support with clinical and radiological assessment.

Most osteoarthritis patients will report a significant improvement in their pain, range of motion and quality of life following an anterior hip replacement. Melbourne patients prefer this approach for its faster recovery time and effectiveness.
Frequently Asked Questions About Hip Replacement?
What Is The Process Moving Forward?
Step 1: Book A Consultation
If you do require surgery, we will schedule and walk you through the process of your operation.
Step 2 Schedule Surgery
During your appointment, Dr Parminder Singh will take a history, examine you and review the relevant radiology. If any further scans are required Dr Singh will request those. Once the diagnosis has been confirmed Dr Singh will discuss the non-surgical option and surgical options of surgery. If no surgery is required Dr Singh may refer you to a physiotherapist for non-surgical management. If surgery is required Dr Singh will consent you for the surgery explained the risk and benefits of the procedure and the expected outcome.
Step 3 Surgery
Dr Parminder Singh will see you before the surgery in the waiting bay and ensure all your questions have been answered prior to surgery.
Dr Parminder Singh will examine your hip, thigh and leg making sure there are no open wounds or signs of skin infection.
If there are any signs of infection, you surgery will be cancelled and rescheduled for another day. Once this has been check Dr Parminder Singh will draw an arrow on the side of your thigh confirming with you the side of surgery. Dr Parminder Singh will check your consent form to again confirm the operation being performed and side of surgery.
Step 4 Recovery
Following your surgery, you will recover on the ward. Most individual stay three to four nights in the hospital and will be seen by the physiotherapist on the ward to facilitate mobilisation using crutches for the first 1-2 weeks.
Some individuals will use the crutches for longer depending on the type of injury and treatment required. Dr Parminder Singh will see you in his rooms approximately 10-14 days after the hip replacement surgery and inspect the hip wound.
The stitches will be removed during this appointment. Dr Parminder Singh will also explain the operative findings and recommended precautions and rehabilitation required. Another appointment will typically be organised for you around 6-8 week after this date to assess your progress. In the meantime, rehabilitation is usually recommended with a physiotherapist who has experience with hip replacement patients.
It is important to follow the hip precautions Dr Parminder Singh recommends to allow for the best possible outcome.
Further appointments will be made at approximately 6 and 12months post operatively and check x-rays will be requested. Dr Parminder Singh recommends to allow approximately 3 months for the soft tissue healing from the surgery and hip precautions during this period. The bone healing will continue for up to 12 months after surgery and Dr Singh will check this for you during the following up appointments. In terms of longer term, Dr Singh will review you in 5, 10, 15, 20 years after your hip replacement with regular x-rays.
Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
Brighton VIC 3186
Book a consultation on:
(03) 9428 4128
Boxhill VIC 3128
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
Blanton Dr,
Mulgrave VIC 3170
Book a consultation on:
(03) 9428 4128
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Book a Consultation
Committed to improving the quality of patient advice, treatment and care in the field of orthopaedics, book a one-on-one consultation with Dr Parminder J Singh today.


