Types of Fractures
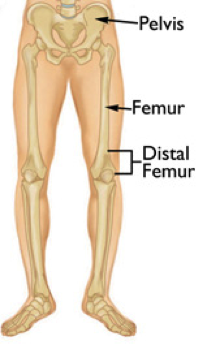
DISTAL FEMUR (THIGH BONE) FRACTURES OF THE KNEE
A fracture is a broken bone. Fractures of the thighbone that occur just above the knee joint are called distal femur fractures. The distal femur is where the bone flares out like an upside-down funnel.
Distal femur fractures most often occur either in older people whose bones are weak, or in younger people who have high energy injuries, such as from a car crash. In both the elderly and the young, the breaks may extend into the knee joint and may shatter the bone into many pieces.
CAUSE
Fractures of the distal femur most commonly occur in two patient types: younger people (under age 50) and the elderly.
Distal femur fractures in younger patients are usually caused by high energy injuries, such as falls from significant heights or motor vehicle collisions. Because of the trauma involved in these fractures, many patients also have other injuries, often of the head, chest, abdomen, pelvis, spine, and other limbs.
Elderly people with distal femur fractures typically have poor bone quality. As we age, our bones get thinner. Bones can become very weak and fragile. A lower-force event, such as a fall from standing, can cause a distal femur fracture in an older person who has weak bones. Although these patients do not often have other injuries, they may have concerning medical problems, such as conditions of the heart, lungs, and kidneys, and diabetes.
SYMPTOMS
The most common symptoms of distal femur fracture include:
- Pain with weight-bearing
- Swelling and bruising
- Tenderness to touch at fracture site
- Deformity — the knee may look “out of place” and the leg may appear shorter and crooked
In most cases, these symptoms occur around the knee, but you may also have symptoms in the thigh area.
TREATMENT
They are non-surgical (Casting and bracing) and surgical treatments that exist for this fracture.
Because of newer techniques and special materials, the results of surgical treatment are good, even in older patients who have poor bone quality.
RECOVERY
A distal femur fracture is a severe injury. Depending on several factors — such as your age, general health, and the type of fracture you have — it may take a year or more of rehabilitation before you are able to return to all everyday activities.
EARLY MOTION
Your doctor will decide when it is best to begin moving your knee in order to prevent stiffness. This depends on how well the soft tissues (skin and muscle) are recovering and how secure the fracture is after having been fixed.
WEIGHT-BEARING
To avoid problems, it is very important to follow your doctor’s instructions for putting weight on your injured leg.
Whether your fracture is treated with surgery or not, your doctor will most likely discourage weight-bearing until some healing has occurred.
REHABILITATION
When you are allowed to put weight on your leg, it is very normal to feel weak, unsteady, and stiff. Even though this is expected, be sure to share your concerns with your doctor and physical therapist. A rehabilitation plan will be designed to help restore normal muscle strength, joint motion, and flexibility.
PATELLAR (KNEECAP) FRACTURES
Because your kneecap (patella) acts like a shield for your knee joint, it can easily be broken. Falling directly onto your knee, for example, is a common cause of patellar fractures.
These fractures can be treated either in a brace or with surgery depending on the severity of the injury. Over the long term, some injuries to the patella are at increased risk of developing arthritis in the knee.
CAUSE
Patellar fractures are most commonly caused by a direct blow, such as from a fall or motor vehicle collision. The patella can also be fractured indirectly. For example, your thigh muscles can contract so violently that it pulls the patella apart.
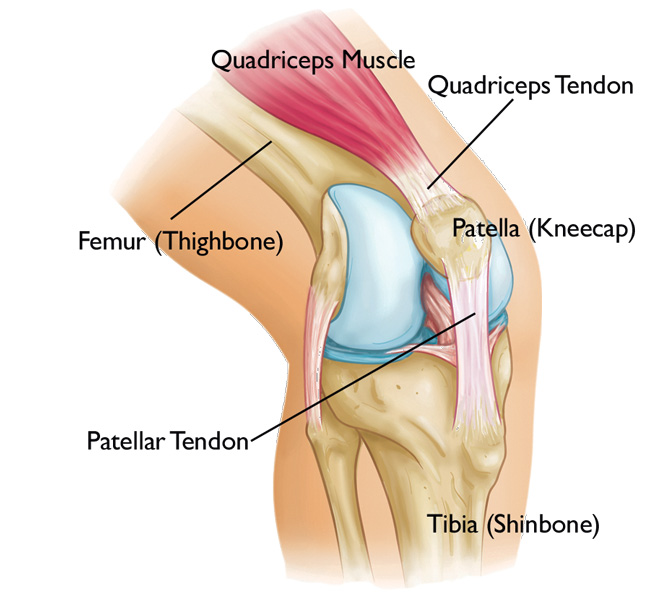
ANATOMY
The patella is a small bone located in front of your knee joint — where the thigh bone (femur) and shinbone (tibia) meet. It protects your knee and connects the muscles in the front of your thigh to your tibia.
The ends of the femur and the undersides of the patella are covered with a slippery substance called articular cartilage. This helps the bones glide smoothly along each other as you move your leg.
SYMPTOMS
The major symptoms of a patellar fracture include pain and swelling in the front of the knee. Additional symptoms include:
- Bruising
- Inability to straighten the knee
- Inability to walk
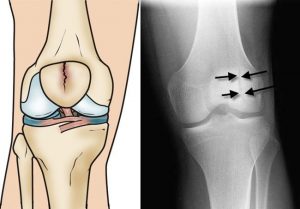
TESTS
X-rays are the most common and widely available diagnostic imaging technique. They create images of dense structures, like bone, so are particularly useful in showing fractures. X-rays are important for showing front and side views of the fracture.
TYPES OF PATELLAR FRACTURES
- Patellar fractures vary. The kneecap can crack just slightly, or can be broken into many pieces.
- A break in the kneecap can happen at the top, centre, or lower part of the bone. Sometimes, fractures occur in more than one area of the kneecap.
- Stable fracture. This type of fracture is non-displaced. The broken ends of the bones meet up correctly and are aligned. In a stable fracture, the bones usually stay in place during healing.
- Displaced fracture. When a bone breaks and is displaced, the broken ends are separated and do not line up. This type of fracture often requires surgery to put the pieces back together.
- Comminuted / Multi-fragmentary fracture. This type of break is very unstable. The bone shatters into three or more pieces.
- Open fracture. In this type of fracture, the skin has been broken and exposes the bone. These injuries often involve much more damage to the surrounding muscles, tendons, and ligaments. Open fractures have a higher risk for complications particular infection and delayed healing.
TREATMENT
NON-SURGICAL TREATMENT
If the pieces of broken bone have not been displaced by the force of the injury, you may not need surgery. Casts or splints may be used to keep your knee straight. This will keep the broken ends in proper position while they heal.
SURGICAL TREATMENT
If the patella has been pulled apart (displaced), you will most likely need surgery. Fractured patellar bones that are not close together often have difficulty healing or may not heal. The thigh muscles that attach to the top of the patella are very strong and can pull the broken pieces out of place during healing.
Procedure: The type of procedure performed often depends on the type of fracture you have. Before the surgery, Dr Parminder J Singh will discuss your procedure with you, as well as any potential risk of complications.
RECOVERY
How long it takes to recover from a patellar fracture will depend on the severity of your injury and whether it required surgery. You will be guided by Dr Parminder J Singh when it is safe to begin putting weight on your leg, and return to work and other activities.
REHABILITATION
Whether your treatment involves surgery or not, rehabilitation plays a vital role in getting you back to your daily activities. Keeping your leg immobilised in a cast can result in knee stiffness and weak thigh muscles. Specific exercises will help strengthen your leg muscles and restore range of motion in your knee.
TIBIAL PLATEAU FRACTURE
Tibial plateau fracture is a bone fracture or break in the continuity of the bone occurring in the proximal part of the tibia or shinbone called the tibial plateau; affecting the knee joint, stability and motion.
SIGNS AND SYMPTOMS
Tibial plateau fractures typically presents with knee effusion, swelling of the knee soft tissues and inability to bear weight. The knee may be deformed due to displacement and/or fragmentation of the tibia which leads to loss of its normal structural appearance. Blood in the soft tissues and knee joint (haemarthrosis) may lead to bruising and a doughy feel of the knee joint. Due to the tibial plateau’s proximity to important vascular (i.e. arteries, veins) and neurological (i.e. nerves such as peroneal and tibial) structures, injuries to these may occur upon fracture. A careful examination of the neurovascular systems is important. A serious complication of tibial plateau fractures is compartment syndrome in which swelling causes compression of the nerves and blood vessels inside the leg and may ultimately lead to necrosis or cell death of the leg tissues. Early diagnosis and treatment can reduce the risk of occurring.
CAUSE
Commonly seen in older females due to osteoporotic bone changes or the result of motor vehicle accidents, falls or sports related injuries.
DIAGNOSIS
In all injuries to the tibial plateau, a combination of x-rays, Magnetic Resonance images (MRI) and CT scan may be necessary. In particular, the MRI are helpful when meniscal, ligamentous and soft tissue injuries are suspected. The CT scan is useful to assess the exact fracture configuration and help decide on the definitive management plan.
TREATMENT AND PROGNOSIS
The goal of therapy is to reduce the fracture and begin early mobilisation.
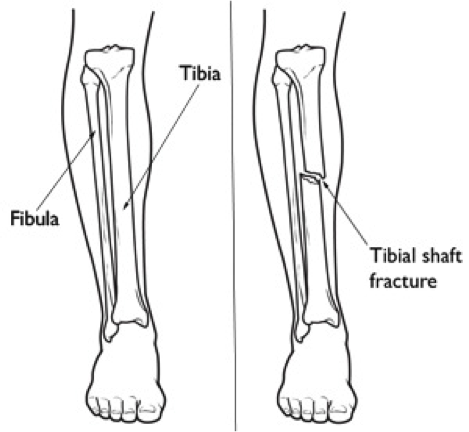
TIBIA (SHINBONE) SHAFT FRACTURES
The tibia, or shinbone, is the most common fractured long bone in your body. The long bones include the femur, humerus, tibia, and fibula. A tibial shaft fracture occurs along the length of the bone, below the knee and above the ankle.
Because it typically takes a major force to break a long bone, other injuries often occur with these types of fractures.
ANATOMY
The lower leg is made up of two bones: the tibia and fibula. The tibia is the larger of the two bones. It supports most of your weight and is an important part of both the knee joint and ankle joint.
TYPES OF TIBIAL SHAFT FRACTURES
The tibia can break in several ways. The severity of the fracture usually depends on the amount of force that caused the break. The fibula is often broken as well.
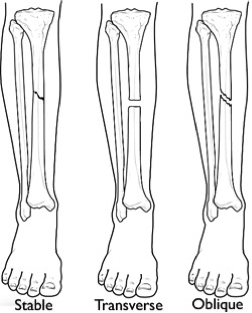
Common types of tibial fractures include:
Stable fracture
This type of fracture is barely out of place. The broken ends of the bones are aligned. In a stable fracture, the bones usually stay in place during healing.
Displaced fracture: When a bone breaks and is displaced, the broken ends are separated and do not line up. These types of fractures often require surgery to put the pieces back together.
Transverse fracture
This type of fracture has a horizontal fracture line. This fracture can be unstable, especially if the fibula is also broken.
Oblique fracture
This type of fracture has an angled pattern and is typically unstable. If an oblique fracture is initially stable or minimally displaced, over time it can become more out of place. This is especially true if the fibula is not broken.
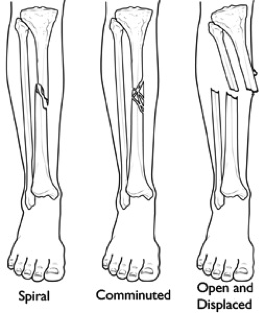
Spiral fracture
This type of fracture is caused by a twisting force. The result is a spiral-shaped fracture line about the bone, like a staircase. Spiral fractures can be displaced or stable, depending on how much force causes the fracture.
Comminuted or Multi-fragmentary fracture
This type of fracture is very unstable. The bone shatters into three or more pieces.
Open fracture
When broken bones break through the skin, they are called open or compound fractures. For example, when a pedestrian is struck by the bumper of a moving car, the broken tibia may protrude through a tear in the skin and other soft tissues.
CAUSE
High-energy collisions, such as an automobile or motorcycle crash, are common causes of tibial shaft fractures. In cases like these, the bone can be broken into several pieces (comminuted / multi-fragmentary fracture).
Sports injuries, such as a fall while skiing or running into another player during soccer, are lower-energy injuries that can cause tibial shaft fractures. These fractures are typically caused by a twisting force and result in an oblique or spiral type of fracture.
SYMPTOMS
The most common symptoms of a tibial shaft fracture are:
- Pain
- Inability to walk or bear weight on the leg
- Deformity or instability of the leg
- Bone “tenting” the skin or protruding through a break in the skin
- Occasional loss of feeling in the foot
DOCTOR EXAMINATION
It is important that your Dr Parminder J Singh knows the circumstances of your injury. For example, if you fell from a tree, how far did you fall? It is just as important for your Dr Parminder J Singh to know if you sustained any other injuries. Your doctor also needs to know if you take any medications.
After the visual inspection, your doctor will feel along your leg to see if there are abnormalities of the tibia. If you are awake and alert, your doctor will test your sensation and muscle strength by asking you to move your toes and see if you can feel different areas over your foot and ankle.
TESTS
X-rays can show if the bone is broken and whether there is displacement (the gap between broken bones). They can also show how many pieces of bone there are. X-rays are also useful for identifying the involvement of the knee or ankle joint, and the presence of a fibula fracture.
After reviewing your x-rays, your Dr Parminder J Singh may recommend a CT scan of your leg. This is often done if there is a question of the fracture extending into either the knee or ankle joint.
TREATMENT
Multiple non-surgical and surgical treatments can be applied depending on the Dr Singh’s prognostic and severity of the fracture.
RECOVERY
How long it takes to return to daily activities varies with different types of fractures. Some tibial shaft fractures heal within 4 months, yet many may take 6 months or longer to heal. This is particularly true with open fractures and fractures in patients who are less healthy.
- Early motion. Dr Parminder J Singh may encourage leg motion early in the recovery period. For example, if soft tissue injury is present with a fracture, the knee, ankle, foot, and toes may be mobilized early in order to prevent stiffness.
- Physical therapy. While you are wearing your cast or splint, you will likely lose muscle strength in the injured area. Exercises during the healing process and after your cast is removed are important. They will help you restore normal muscle strength, joint motion, and flexibility.
- Weight-bearing. When you begin walking, you will most likely need to use crutches or a walker.
It is very important to follow Dr Parminder J Singh’s instructions for putting weight on your injured leg to avoid problems. In some cases, doctors will allow patients to put as much as weight as possible on the leg right after surgery. However, you should always follow the specific directions given by your surgeon.
Fracture pain usually stops long before the bone is solid enough to handle the stresses of everyday activities. If the bone is not healed and you put weight on it too soon, it could fail to heal. If that occurs, you may need a secondary surgical procedure, such as bone grafting or revision fixation.
What Is The Process Moving Forward?
Step 1: Book A Consultation
If you do require surgery, we will schedule and walk you through the process of your operation.
Step 2 Schedule Surgery
During your appointment, Dr Parminder Singh will take a history, examine you and review the relevant radiology. If any further scans are required Dr Singh will request those. Once the diagnosis has been confirmed Dr Singh will discuss the non-surgical option and surgical options of surgery. If no surgery is required Dr Singh may refer you to a physiotherapist for non-surgical management. If surgery is required Dr Singh will consent you for the surgery explained the risk and benefits of the procedure and the expected outcome.
Step 3 Surgery
Dr Parminder Singh will see you before the surgery in the waiting bay and ensure all your questions have been answered prior to surgery.
Dr Parminder Singh will examine your hip, thigh and leg making sure there are no open wounds or signs of skin infection.
If there are any signs of infection, you surgery will be cancelled and rescheduled for another day. Once this has been check Dr Parminder Singh will draw an arrow on the side of your thigh confirming with you the side of surgery. Dr Parminder Singh will check your consent form to again confirm the operation being performed and side of surgery.
Step 4 Recovery
Following your surgery, you will recover on the ward. Most individual stay 3-5 nights in hospital and will be seen by the physiotherapist on the ward to facilitate mobilisation using crutches for the first 6-12 weeks.
Some individuals will use the crutches for longer depending on the type of injury and treatment required. Dr Parminder Singh will see you in his rooms approximately 10-14 days after the surgery and inspect the wound.
The stitches will be removed during this appointment. Dr Parminder Singh will also explain the operative findings and recommended precautions and rehabilitation required. Another appointment will typically be organised for you around 6-8 week after this date to assess your progress with X-rays to assess for fracture healing. In the meantime, rehabilitation is usually recommended with a physiotherapist who has experience with fractures of the lower limb.
It is important to follow the precautions Dr Parminder Singh recommends particle protected weight bearing to allow for the best possible outcomes.
Any further appointment will be made on a case by case basis depending on your condition. In general terms, Dr Parminder Singh recommends approximately 3-8 months for healing from the surgery and will vary based on the individual characteristics of the injury.
Consulting Locations
Richmond VIC 3121
Book a consultation on:
(03) 9428 4128
Brighton VIC 3186
Book a consultation on:
(03) 9428 4128
Boxhill VIC 3128
Book a consultation on:
(03) 9428 4128
343-357 Blackburn Rd,
Mt. Waverley VIC 3149
Book a consultation on:
(03) 9428 4128
Book Online at Waverley Private Hospital
Blackburn VIC 3130
Book a consultation on:
(03) 9428 4128
Book Online at Forest Hill
Gisborne VIC 3437
Book a consultation on:
(03) 9428 4128
Book Online at Gisborne
262 Main St,
Mornington VIC 3931
Book a consultation on:
(03) 9428 4128
Book Online at Mornington
Blanton Dr,
Mulgrave VIC 3170
Book a consultation on:
(03) 9428 4128
108 Bridport Street,
Albert Park VIC 3206
Book a consultation on:
(03) 9428 4128
Book Online at Albert Park
240 Hoppers Lane,
Werribee VIC 3030
Book a consultation on:
(03) 9428 4128
Make an appointment with our Melbourne orthopaedic surgeons
If you are a Melbourne patient suffering from a knee or hip complaint, you can get a referral and make an appointment with a surgeon at PJS Orthopaedics at a time and location that suits you.
Whether your knee or hip injury is a result of playing sport, has come about because of trauma injury, or is simply due to wear and tear, our Melbourne surgeons have the experience and expertise to find a surgery solution that is right for you.


